Managing and Treating Opioid-Induced Constipation
*Please note: This slide show represents a visual interpretation and is not intended to provide, nor substitute as, medical and/or clinical advice.
What is opioid-induced constipation (OIC)?
Opioid-induced constipation (OIC) is a condition that affects how your digestive system works.
Opioids are strong pain medicines that slow bowel movements. This means fewer bowel movements or more difficulty having a bowel movement than normal.1,2 Hence the term "opioid-induced" constipation.
Side effects of opioids
Your physician might prescribe opioids if you have a condition that causes moderate to severe pain.
While opioids can treat pain effectively, they also cause side effects. Between 50 and 80 percent of people who take opioid medicines may have constipation.3
OIC – Most common digestive system side effect of opioids
OIC is the most common side effect that opioids have on your digestive system. However, there are others. Opioid-induced bowel dysfunction (OIBD) is the medical term for all the digestive system effects that opioids can cause. Besides constipation, OIBD can include heartburn, nausea, vomiting, a bloated feeling, as well as chronic, or long-lasting, abdominal pain.
How is OIC managed and treated?
There are different ways to manage and treat OIC. Your physician will probably ask about your diet and lifestyle and recommend non-prescription medicines.3 If these do not work, they might prescribe a different pain medicine or a medicine to treat OIC.
This animation tells you about the possible ways to manage and treat OIC.
Standard of care in OIC management
First of all, your physician should make sure opioid medicines are the best choice for treating your pain when they prescribe them. Next, they should make sure you are taking the lowest dose needed to control your pain.
A physician who specializes in managing pain is an important part of your healthcare team. They can help the physician who is prescribing your opioid medicine find ways to prevent OIC and other side effects, or find ways to lower the risk of OIC.4
Medicines for OIC: Non-prescription laxatives
Taking non-prescription laxative medicines may help you manage OIC. These medicines work in different ways. They can:
- Stimulate the nerves in your digestive system.
- Soften the waste or make it bulkier.
All these things can make it easier to have a bowel movement.4,5
Which laxatives should I take if I have OIC?
You might need to try different types of laxatives, or take more than one. For example, you can take a type of laxative called a "stool softener" that makes your stool easier to pass. Or you can take a type called a "stimulant laxative" that makes the nerves in your digestive system more active and sensitive. This can get your digestive system moving again.
What types of non-prescription laxatives are available to treat OIC?
Your physician may recommend you take both types or another type of laxative. Polyethylene glycol is another type that may help. Your physician can help you decide which laxatives work best and how much you'll need to take.
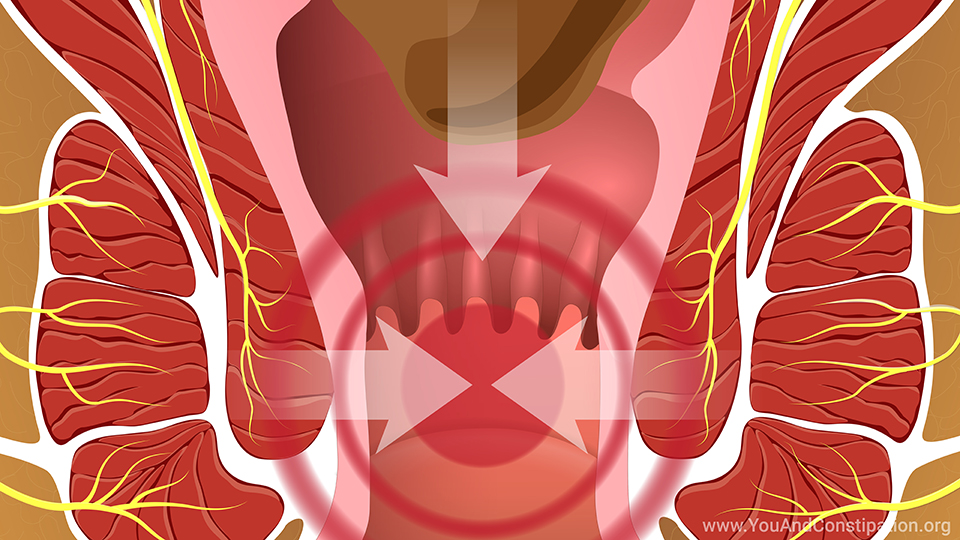
Do people with OIC have risks for other disease conditions?
You may need prescription medicines to treat OIC because it can cause health problems. For example, straining to have a bowel movement could cause hemorrhoids and pain and burning in the rectum and anal area. The rectum is where stool is stored before it leaves the body, and the anus is where it comes out.
Prescription medicines for OIC: Lubiprostone
If laxatives do not help your OIC, you may need prescription medicines. A medicine called lubiprostone helps more water enter the digestive system. This medicine relieves OIC for some people.4
Prescription medicines for OIC: Methylnaltrexone bromide
Some medicines keep opioids from attaching to the receptors in your digestive system and slowing it down. These medicines are called "opioid antagonists." They "fight" the normal action of the opioids in your intestines without affecting pain control.
A medicine called methylnaltrexone bromide is this type.4
Other medicines that block opioids in the digestive system
Naloxegol and naldemidine are two other medicines that block the effects of opioids on the digestive system. Your physician can talk with you about whether any of these medicines is right for you.
Are there alternative medicines to opioids?
If you develop opioid-induced constipation, changing your pain medicine is one option. This can control pain while relieving constipation. Your physician might prescribe a non-opioid medicine or lower your opioid dose.5
Alternative opioid medicines: Naloxone
Naloxone is a medicine that might help prevent OIC.5 It contains an opioid and a medicine that blocks the usual effects of opioids on your digestive system.7 So it may reduce constipation.
Questions to ask your physician about OIC treatment
Tell your physician if you have constipation when taking opioid medicines. If one way of treating constipation does not work, ask what else you can try. This might include switching to a different pain medicine. Your physician can help you find the best way to control pain and avoid constipation.
References
- About constipation. International Foundation for Gastrointestinal Disorders. Available at https://www.aboutconstipation.org/. Accessed December 2019.
- Ford AC, Moayyedi P, Lacy BE, et al. American College of Gastroenterology monograph on the management of irritable bowel syndrome and chronic idiopathic constipation. Am J Gastroenterol 2014;109(S1):S2-S26.
- Poulsen JL, Brock C, Olesen AE, et al. Evolving paradigms in the treatment of opioid-induced bowel dysfunction. Therap Adv Gastroenterol 2015;8(6):360-372.
- Crockett SD, Greer KB, Heidelbaugh JJ, et al. American Gastroenterological Association Institute guidelines on the medical management of opioid-induced constipation. Gastroenterology 2019;156:218-226.
- Kumar L, Barker C, Emmanuel A. Opioid-induced constipation: Pathophysiology, clinical consequences, and management. Gastroenterol Res Pra 2014;2014:141737.
- Drewes AM, Munkholm M, Simrén M, et al. Definition, diagnosis and treatment strategies for opioid-induced bowel dysfunction—Recommendations of the Nordic Working Group. Scand J Pain 2016;11:111-122.
- Understanding naloxone. Harm Reduction Coalition. Available at https://harmreduction.org/issues/overdose-prevention/overview/overdose-basics/understanding-naloxone/. Accessed December 2019.
- Müller-Lissner S, Bassotti G, Coffin B, et al. Opioid-induced constipation and bowel dysfunction: A clinical guideline. Pain Med 2017;18(10):1837-1863.
- Gudin J, Fudin J. Opioid-induced constipation: New and emerging therapies – Update 2016. Practical Pain Management 2016;16(10). Available at https://www.practicalpainmanagement.com/treatments/pharmacological/non-opioids/opioid-induced-constipation-new-emerging-therapies-update?page=0,3. Accessed December 2019.
This slide show provides an overview of possible ways to
manage and
treat opioid-induced constipation (
OIC). Your physician will probably ask about your diet and lifestyle and recommend non-prescription laxative medicines. If these do not work, they might prescribe a different pain medicine or a medicine to treat OIC. The animation describes lubiprostone, methylnaltrexone bromide, as well as medicines that block opioids in the digestive system, and alternative medicines to opioids. Tell your physician if you have constipation when taking opioid medicines. Your physician can help you find the best way to control pain and avoid constipation.
-
Share with family and friends:
Click here to take our SURVEY
Your feedback is important to us! We will use your feedback to develop future areas of content about constipation which will help other patients, caregivers and families.